What Is the Last Stage of Ventilator? Understanding the Critical Phase
What is a Ventilator and Its Purpose?
A ventilator is a life-saving medical device used primarily for patients who are unable to breathe on their own due to severe illness or injury. It takes over the role of breathing by delivering oxygen to the lungs and removing carbon dioxide. Ventilators are commonly used in intensive care units (ICUs) and during surgeries where patients need support for their respiratory systems.
When we talk about the last stage of a ventilator, it's crucial to understand that this stage typically refers to the weaning process—the gradual reduction of ventilator support as the patient’s breathing improves. I remember a time when a family member was on a ventilator due to a severe lung infection, and the doctors explained how delicate this transition can be. It’s not just about turning off the machine—it’s about ensuring the patient’s lungs can take over on their own.
The Weaning Process: The Last Stage of Ventilator Support
What Does Weaning Mean?
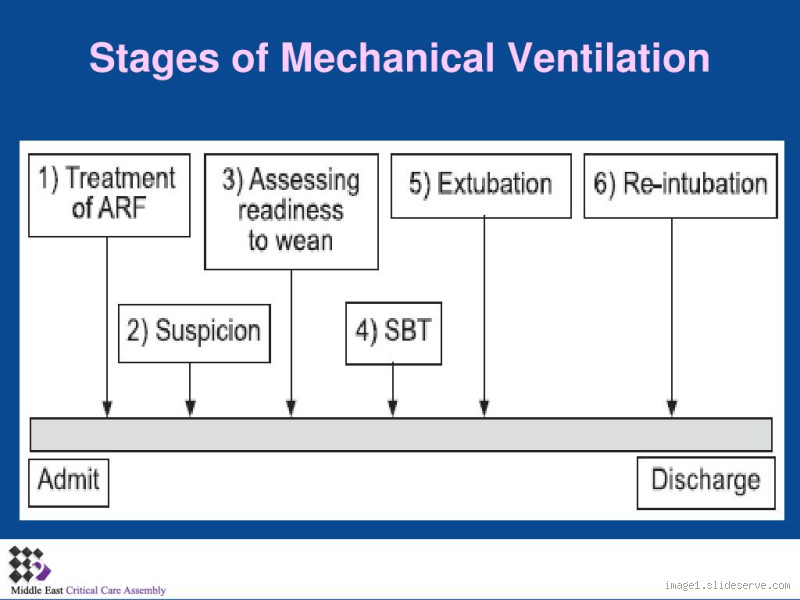
Weaning from a ventilator means gradually reducing the assistance the machine provides, allowing the patient's body to start breathing on its own. The goal is to eventually remove the ventilator completely without compromising the patient’s ability to breathe unaided. This phase is often the final stage of ventilator use before the patient is fully extubated (removed from the ventilator tube).
Weaning is typically performed in stages and requires careful monitoring. Some patients may require a slow, step-by-step reduction in ventilator support, while others may adjust more quickly. The decision to start weaning depends on the patient’s overall health, the reason they were on the ventilator, and their progress during their stay in the ICU.
Phases of Weaning
Spontaneous Breathing Trial (SBT): In this stage, the patient is allowed to breathe on their own for short periods, usually while still attached to the ventilator but with minimal support. If the patient does well, they may progress to further trials. This is a big milestone and often a sigh of relief for both patients and doctors.
Reduced Support: The next phase involves decreasing the pressure or volume of air delivered by the ventilator. This allows the patient’s lungs to do more of the work, while the ventilator still provides assistance if needed.
Extubation: This is the final step, where the ventilator is removed entirely. The patient must be able to breathe independently and maintain stable oxygen levels without mechanical assistance. It’s an intense moment that marks the transition to recovery.
How Do Doctors Decide When to Start Weaning?
Deciding when to begin weaning is a complex process. Doctors evaluate a variety of factors, such as:
Lung function: Can the patient’s lungs effectively oxygenate the blood without assistance?
Strength of respiratory muscles: Are the patient’s muscles strong enough to handle breathing on their own?
Underlying conditions: For example, patients with chronic conditions like COPD or severe pneumonia may take longer to wean off the ventilator.
I recall a friend who was on a ventilator for several days after a car accident. The doctors started weaning him slowly because his lungs weren’t strong enough initially. But after a few tests and trials, he was able to breathe on his own again. It’s a nerve-wracking but ultimately hopeful phase.
Challenges of the Last Stage: Ventilator Weaning
Respiratory Muscle Fatigue
One of the major challenges of the weaning process is respiratory muscle fatigue. Even after being on the ventilator for a short time, the muscles responsible for breathing can weaken. If a patient isn’t able to breathe efficiently on their own, they may need to go back on the ventilator temporarily. This can be frustrating, but it's important to remember that it's a delicate balance.
A recent conversation with a colleague who works in the ICU gave me insight into how often patients need additional support during this phase. It made me realize that while the process of coming off a ventilator seems straightforward, it requires constant attention and patience.
Psychological and Emotional Stress
There’s also a psychological component to weaning. Patients may experience anxiety, stress, or even feelings of claustrophobia as they adjust to breathing on their own again. Being on a ventilator can feel like a lifeline, and the idea of being disconnected can cause distress. It's crucial for healthcare providers to support patients emotionally as well as physically during this transition.
What Happens If Weaning Isn’t Successful?
Ventilator Dependency
For some patients, weaning might not be successful. This can be due to a number of reasons, such as an underlying chronic disease, poor lung function, or inadequate recovery. In these cases, the patient may remain dependent on the ventilator for longer or need to transition to long-term ventilation support.
The possibility of long-term dependence on a ventilator is a difficult reality. It’s important for families and healthcare teams to work together, considering all options for the patient’s future care. I remember hearing a doctor explain to a family how some patients might need a tracheostomy, where a tube is inserted into the windpipe for long-term ventilation. It's a tough decision, but it's part of managing critical conditions.
Conclusion: The Critical Final Stage
In conclusion, the last stage of ventilator support is the weaning process, and it’s a critical part of recovery for patients who’ve relied on mechanical breathing support. It’s a process that requires careful monitoring, patience, and expertise from medical professionals. Although it can be a challenging phase, the goal is always to give the patient the best chance of recovery and independence from the ventilator.
If you or someone you know is undergoing this process, understanding what happens during the weaning phase can help manage expectations and provide clarity during a difficult time. The hope is always to reach a point where the patient is able to breathe independently, marking the end of a challenging but essential medical journey.
How much height should a boy have to look attractive?
Well, fellas, worry no more, because a new study has revealed 5ft 8in is the ideal height for a man. Dating app Badoo has revealed the most right-swiped heights based on their users aged 18 to 30.
Is 172 cm good for a man?
Yes it is. Average height of male in India is 166.3 cm (i.e. 5 ft 5.5 inches) while for female it is 152.6 cm (i.e. 5 ft) approximately. So, as far as your question is concerned, aforesaid height is above average in both cases.
Is 165 cm normal for a 15 year old?
The predicted height for a female, based on your parents heights, is 155 to 165cm. Most 15 year old girls are nearly done growing. I was too. It's a very normal height for a girl.
Is 160 cm too tall for a 12 year old?
How Tall Should a 12 Year Old Be? We can only speak to national average heights here in North America, whereby, a 12 year old girl would be between 137 cm to 162 cm tall (4-1/2 to 5-1/3 feet). A 12 year old boy should be between 137 cm to 160 cm tall (4-1/2 to 5-1/4 feet).
How tall is a average 15 year old?
Average Height to Weight for Teenage Boys - 13 to 20 Years
| Male Teens: 13 - 20 Years) | ||
|---|---|---|
| 14 Years | 112.0 lb. (50.8 kg) | 64.5" (163.8 cm) |
| 15 Years | 123.5 lb. (56.02 kg) | 67.0" (170.1 cm) |
| 16 Years | 134.0 lb. (60.78 kg) | 68.3" (173.4 cm) |
| 17 Years | 142.0 lb. (64.41 kg) | 69.0" (175.2 cm) |
How to get taller at 18?
Staying physically active is even more essential from childhood to grow and improve overall health. But taking it up even in adulthood can help you add a few inches to your height. Strength-building exercises, yoga, jumping rope, and biking all can help to increase your flexibility and grow a few inches taller.
Is 5.7 a good height for a 15 year old boy?
Generally speaking, the average height for 15 year olds girls is 62.9 inches (or 159.7 cm). On the other hand, teen boys at the age of 15 have a much higher average height, which is 67.0 inches (or 170.1 cm).
Can you grow between 16 and 18?
Most girls stop growing taller by age 14 or 15. However, after their early teenage growth spurt, boys continue gaining height at a gradual pace until around 18. Note that some kids will stop growing earlier and others may keep growing a year or two more.
Can you grow 1 cm after 17?
Even with a healthy diet, most people's height won't increase after age 18 to 20. The graph below shows the rate of growth from birth to age 20. As you can see, the growth lines fall to zero between ages 18 and 20 ( 7 , 8 ). The reason why your height stops increasing is your bones, specifically your growth plates.
